Introduction
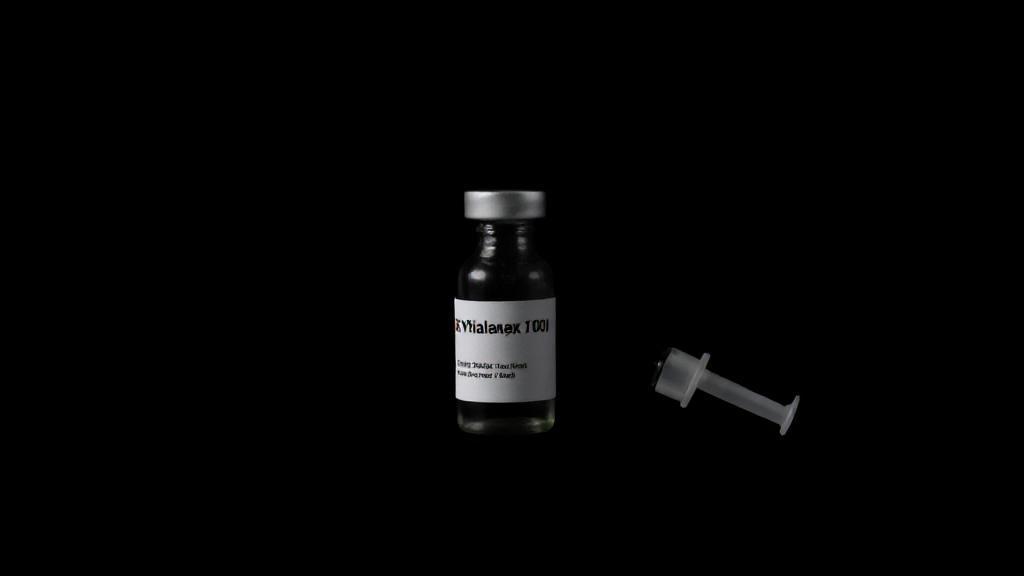
In recent years, a powerful sedative known as "Tranq" or "zombie drug" has emerged as one of the most alarming developments in the ongoing drug crisis. Xylazine, a non-opioid veterinary tranquilizer, has infiltrated the illicit drug market, raising significant concerns among health professionals and law enforcement agencies. Originally developed for veterinary use, xylazine is now being misused by humans, leading to dangerous and sometimes fatal consequences.
What is Xylazine?
Xylazine is a non-opioid sedative, analgesic, and muscle relaxant primarily used in veterinary medicine to sedate large animals such as horses and cattle. First synthesized in 1962 by Bayer, it is not approved for human use by the U.S. Food and Drug Administration (FDA).
Chemical Composition
The chemical formula for xylazine is C12H16N2S, and it belongs to the class of drugs known as alpha-2 adrenergic agonists. This class of drugs works by inhibiting the release of norepinephrine and dopamine, leading to sedation and muscle relaxation.
The Growing Crisis
Recent data from the Drug Enforcement Administration shows alarming statistics:
- 40% of street drugs tested in Philadelphia contained xylazine
- 25% increase in xylazine-related deaths nationwide from 2020 to 2021
- Present in over 30 states' drug supplies
Health Impacts and Risks
Immediate Effects
- Extreme sedation
- Respiratory depression
- Dangerously low blood pressure
- Decreased heart rate
- Mental confusion
Long-term Consequences
One of the most distinctive and troubling effects of xylazine is the development of severe skin ulcers. These wounds:
- Appear even when the drug is injected at other sites
- Are highly resistant to traditional wound care
- Can lead to amputation if left untreated
- May persist even after drug use stops
Treatment Challenges
"The introduction of xylazine into the drug supply has complicated an already devastating overdose crisis." - Dr. Rahul Gupta, Director of National Drug Control Policy
Traditional overdose reversal medications like naloxone (Narcan) don't work on xylazine because it's not an opioid. While naloxone should still be administered in suspected overdoses due to common mixing with fentanyl, additional medical intervention is typically necessary.
Prevention and Support
For Healthcare Providers
- Enhanced screening protocols
- Specialized wound care training
- Recognition of xylazine-specific symptoms
Treatment Options
- Medical detoxification to safely manage withdrawal symptoms
- Behavioral therapies such as counseling and support groups
- Medication-Assisted Treatment (MAT) adapted for xylazine misuse
Looking Forward
Researchers at the National Institute on Drug Abuse are working to develop targeted treatments for xylazine exposure. Current initiatives include:
- Enhanced drug supply monitoring
- Development of xylazine-specific test strips
- Implementation of specialized wound care protocols
- Community education programs
Conclusion
The emergence of xylazine represents a new chapter in the substance use crisis, requiring innovative approaches to treatment and prevention. For more information on substance abuse and treatment options, resources such as the Substance Abuse and Mental Health Services Administration (SAMHSA) can provide valuable support and guidance. By staying informed and advocating for effective policies, we can work towards reducing the harm caused by this dangerous substance.
Understanding the risks associated with xylazine is essential for both individuals and communities. As research continues and awareness grows, healthcare providers and harm reduction organizations must adapt their strategies to address this evolving threat to public health.